Functional Load Transfer through the Pelvic Girdle: an Overview of the Research Applicable to the Stork (One Leg Standing) Test
Dr Barbara Hungerford PhD, B App Sci (Physiotherapy)
Introduction
Posterior pelvic girdle pain (PGP) occurs in a variety of population groups, from postpartum women to sports people, as a result of trauma,or injury at work. It is estimated that sacroiliac joint (SIJ) pain occurs in over 15% of people classified as having nonspecific low back pain1, and yet there are presently few reliable diagnostic procedures to assist clinical evaluation of impaired pelvic girdle function2 and resultant PGP.
The articular surfaces of the SIJ assist load transfer from the lumbar spine, through the pelvis, to the lower limbs by way of their shape and alignment3. Research has shown that small amounts of movement occur at the SIJ, and that this movement is controlled during load transfer by engaging the self-bracing mechanism of the SIJ4,5. The self-bracing mechanism is induced by pre-activation of the local muscle system of the lumbo-pelvic region prior to movement6, with subsequent tensioning of the pelvic ligaments and thoraco-lumbar fascia, and compression of the joint surfaces4,7. During activities that induce load transferthrough the pelvis, for example moving from standing to standing on one leg, or lying to standing, a concurrent pattern of sacral nutation, or relative posterior rotation of the innominate engages the SIJ into its closed pack position4,8.
As a clinician, understanding normal biomechanics of the pelvic girdle assisted rehabilitation of PGP patients to a degree, however in the mid 1990’s I felt further research into pelvic biomechanics and muscle recruitment was required to understand the effects of impaired pelvic girdle function. In order to investigate intra-pelvic motion in a minimally invasive fashion, a high resolution motion analysis system using skin mounted markers was chosen to acquire the kinematic data of pelvic bone motion during a standing hip flexion movement. The main emphasis of these studies became investigation of the patterns of bone motion rather than the range of motion, and the temporal relationship of muscle recruitment in the lumbo-pelvic region.
Methods for Intra-pelvic motion and muscle recruitment analysis during the Stork (One Leg Standing) Test
A detailed description of the methods has been published previously6,8 . Fourteen male subjects with pain in the posterior pelvic/ SI region, and a mean (range) age, height and weight of 32.7 (24-47) years, 176.8 (168-184) cm, and 77.0 (71-90) kg respectively, volunteered for the study. All PGP subjects reported unilateral symptomsthat were aggravated by weight bearing activities.All subjects had positive assessment results on the side of posterior pelvic pain in clinical tests for impaired lumbo-pelvic stabilization, that is, they tested positive to the ASLR, Stork and Passive Joint Glide tests on the side of their pain. The PGP group were age and height matched to a control group of fourteen males who had no history of low back pain in the last twelve months, no history of congenital lumbar or pelvic anomalies, and tested negative to the ASLR, Standing hip flexion and Passive Joint Glide tests6.The pattern of relative motion between the innominate and the sacrum, and the innominate and femur, was measured concurrently with surface EMG data recorded from seven trunk and hip muscles on the side of single leg support.
Overview of results from the analysis of Intra-pelvic motion and muscle recruitment during the Stork (One leg Standing) Test
When subjects with no history of lumbo-pelvic pain flexed their hip in standing, the onset of the lower fibres of obliquus internus abdominis(OI) and lumbar multifidus EMG activity on the side
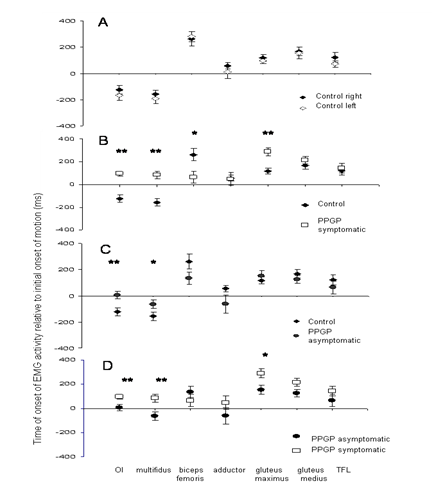
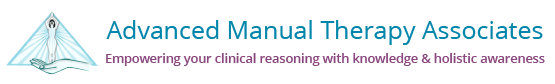
Figure 1:Mean time of EMG onset for the supporting leg during hip flexion in standing in 1A: control subjects; 1B: control subjects versus PGP subjectson the symptomatic side; 1C: control subjectsversus PGP subjects on the asymptomatic side; 1D: asymptomatic versus symptomatic side in PGP subjects. *p £ 0.05; **p £ 0.01. (Reproduced with permission from © AMTA P/L).
of standing on one leg occurred prior to initiation of the task (Fig.1A). In contrast, the onset of biceps femoris, adductor longus, gluteus maximus, gluteus medius, and TFL EMG occurred after initiation of motion. There was no significant difference in onset of EMG activity between sides in control subjects for all seven muscles (Fig.1A)6.
Investigation of motion between the innominate and sacrum on the side of single leg support occurred simultaneously with analysis of EMG activity. The innominate on the side of single leg support posteriorly rotated relative to the sacrum in the control subjects (Fig.2A). A concurrent pattern of side flexion of the innominate toward, and rotation about the vertical axis away from the side of hip flexion also occurred. The weight bearing innominate translated posteriorly, superiorly and medially (toward the sacrum)8.
In comparison to the control subjects, the EMG onsets of OI, multifidus, and gluteus maximus were significantly delayed (p£ 0.01) on the symptomatic side in subjects with PGP (Fig.1B). The onset of OI and multifidus EMG occurred more than 20ms after onset of motion. In contrast, onset of bicep femoris EMG occurred significantly earlier (p< 0.03) on the symptomatic side, in comparison to controls (Fig.1B). When onset of EMG activity on the symptomatic side was compared to the asymptomatic side in the PGP group, there was a significant delay in the onset of activation in OI, multifidus, and gluteus maximus on the symptomatic side (Fig.1D)6.
The pattern of intra-pelvic bone motion was also shown to reliably alter in the presence of PGP. The innominate rotated anteriorly relative to the sacrum on the symptomatic side (Fig.2B), indicative of failure of the self bracing mechanism to maintain the SIJ in its closed pack position. The contralateral patterning of sideflexion and rotation did not alter to the pattern found in controls. The pattern of translation did alter however, with posterior, inferior, and medial translation of the sacrum occurring in subjects with PGP8.
Implications of analysis of the biomechanics and muscle recruitment patterns occurring during the Stork Support test
During the Stork Support test the weight bearing limb maintained single leg support as the non-weight bearing leg moved into hip and knee flexion. Simultaneous analysis of intra-pelvic motion and muscle recruitment patterns in control subjects and subjects with PGP showed that significant differences occurred between these groups.
Control Subjects
Thereported studies were not able to determine whether activation of the horizontally aligned fibres of IO, and lumbar multifidus occurred prior to initiation of the self-bracing mechanism of the SIJ, however they did indicate that the lower fibres of IO, and lumbar multifidus on the side of single leg support activated prior to initiation of motion, and as single leg support occurred, the innominate moved toward posterior rotation relative to the sacrum. This muscle recruitment pattern is consistent with previous research that has identified feedforward activation of transversus abdominis (TrA), OI and multifidus in association with limb movements that
Figure 2: Relative motion between the innominate and sacrum.2A: A depiction of posterior rotation relative to the sacrum expected during single leg support in control subjects. 2B: Anterior rotation of the innominate relative to the sacrum occurs in the presence of PGP during single leg support(Reproduced with permission from © AMTA P/L)
Challengethe stability of the spine 11,12. Previous studies have suggested that TrA and the lower, horizontally oriented fibres of OI, may contribute to compression of the SIJ13 . Similarly, lumbar multifidus activation may increase tension onposterior SI ligaments and posterior layer of the thoraco-lumbar fascia, and induce a nutation force on the sacrum14. We can theorise therefore that pre-activation of the horizontally aligned fibres of the deep abdominal wall and multifidus, as determined in this study, may have contributed to compression of the SIJ prior to initiation of single leg stance, and influenced the motion pattern between the innominate and sacrum as the self bracing mechanism was initiated for optimal pelvic stabilisation and load transference15.
Subjects with PGP
In the PGP group the onset of OI, multifidus, gluteus maximus, and bicep femoris EMG was significantly delayed on the symptomatic side compared to the asymptomatic side, and compared to control subjects. This altered pattern of activation occurred simultaneously with an altered pattern of intra-pelvic bone motion, as anterior rotation of the weight bearing innominate occurred relative to the sacrum.
The delayed onset of the lower fibres of OI and multifidus would suggest a change in the motor control strategy on the symptomatic side in subjects with PGP, with the delayed activation possibly diminishing the effectiveness of stabilising mechanisms at the SIJ prior to increased vertical loading through the pelvis. Delayed activation of gluteusmaximus may have also altered compression of the SIJ. This may therefore have effected the PGP groups’ capacity to maintain alignment of the innominate and sacrum in the self braced position. Vleeminget al15has suggested that anterior rotation of the innominate (sacral counternutation) disengages the self-bracing mechanism of the pelvis and consequently diminishes the ability to transfer loads between the spine and legs. The early onset of bicep femoris activation on the symptomatic side may have occurred to augment force closure across the SIJ via connections to sacrotuberous ligament and the posterior layer of thoraco-lumbar fascia16.
Clinical Implications and Investigation of Intra-therapist reliability to palpate bone motion during the Stork Support test
Posterior rotation of the weight bearing innominate occurred about the coronal axis in control subjects. This pattern reliably altered in subjects with PGP, as anterior rotation of the innominate occurred with load transfer. As the difference in the pattern of bone motion directly reflected the ability (posterior rotation), or inability (anterior rotation), of subjects to maintain pelvic stability for load transfer through the pelvis, Lee17has suggested that the Stork (OLS) test (Figure 3) may provide a useful tool for clinical evaluation of a subjects ability to stabilise intra-pelvic motion. The range of palpable motion between the innominate and sacrum is, however, small5,8, and this may effect the ability and reliability of clinicians to palpate pelvic bone motion in vivo.
Application of the Stork (OLS) test involves palpation of the PSIS and innominate on the side of the pelvis to which weight is to be transferred for single leg support, while the therapists other hand palpates centrally on the sacrum at S2. The direction of bone motion, or lack of bone motion, is then palpated as the contralateral foot is lifted off the ground (Fig.3). Clinically, the results have either been described by the direction of PSIS movement (cephalad, caudad, or no movement relative to S2) occurring with innominate motion, or as a positive or negative result. In the second description, a negative result is when no relative motion between the innominate and sacrum is palpated (Fig.3A), while cephalad motion of the PSIS relative to the sacrum (Fig.3B) is considered positive17.
A study of inter-therapist reliability to palpate innominate motion relative to the sacrum during the Stork Support test was undertaken as the first stage of considering the clinical application of this test18.


Fig. 3A Fig. 3B
Figure 3:Subject palpation for the Stork test on the support side. A: A negative right support side test. B: A positive left support side test with cephalad motion of the left PSIS relative to S2 central.
Methods
A detailed description of the methods has been published previously18.Thirty three subjects aged 36.2 ± 13.4 yearsparticipated in the study. There were no exclusion criteria except that subjects must have been over 18 years. The subjects varied in gender, history of back or leg pain in the previous 12 months, and presence of pain at the time of testing. Eleven female and four male subjects were symptomatic (VAS > 0) at the time of testing. There were no subjects who reported that they were pregnant at the interview.
Three experienced manual therapists (mean 14.7 years, range 7- 21 years in practice; age range 37 -42 years) were included in the study as they regularly used the Stork Support test as part of their assessment protocols. Explanation of the Stork Support test has been published fully18. The test movement was repeated three times on the right and then performed on the left.
The therapists graded the test according to 2 scales. In Part 1 the therapist was asked to rate the direction of intra-pelvic motion using a 3 point scale where the PSIS either moved cephalad relative to the sacrum, the PSIS stayed neutral, or the PSIS moved caudally relative to the sacrum. In Part 2 the therapist was asked to rate the direction of intra-pelvic motion using a 2 point scale, being positive if the PSIS moved cephalad relative to the sacrum, or negative if the PSIS stayed neutral or moved caudal relative to the sacrum.
Inter-rater reliability was assessed using a Cohen kappa reliability coefficient (k). Manual calculation of k for more than two therapists was done according to Pittenger19 and interpreted as poor (<0.2); fair (0.21-0.40); moderate (0.41-0.60; good (0.61-0.80) and excellent (0.81-1.0). Percent close agreement (PCA) was calculated to assess agreement between therapists.
Results Overview
When therapists were asked to rate the direction of intra-pelvic motion as positive or negative (a 2 point scale) the inter-rater reliability was goodfor both the left and right sides (Left k = 0.67 and Right k = 0.77). 100% agreement between raters was seen for 91.9% and 89.9% of the time for the left and right sides respectively. Again Pearson’s Chi Square (c2) test of association showed that gender, back-pain in last 12 months, leg-pain in last 12 months, and present pain as assessed using a McGill questionnaire, VAS and PPI, had no association on the therapist’s ratings. Inter-rater reliability for the 3-point scale showed moderate reliability for both the left and right sides (Left k = 0.59 and Right k = 0.59), with the percentage of agreement decreasing to 82.8% (left) and 79.8% (right).
Discussion
When using a 2-point scale to determine a negative or positive result in the Stork Support test the inter rater reliability was good for both sides and the Percentage Close Agreement was high. The results suggest that multiple therapists have good reliability for determining a positive or negative result in the Stork Support test. Application of the Stork Support test will be more reliable if clinicians describe their palpation as either a negative result, that is, no relative movement between the innominate and sacrum, or a positive result (cephalad motion of the PSIS relative to the sacrum). Increasing the choices by describing the direction of intra-pelvic motion is only likely to decrease the inter-rater reliability of the test.
In normal function minimal intra-pelvic motion should occur between the innominate and sacrum during a weight bearing task such as standing on one leg, due to compression of the articular surfaces with activation of the self-bracing mechanism4,15. In the 2 point scale of the Stork Support test, this normal function would be indicated as a negative test. A positive test would suggest an inability of the SIJ to engage the self bracing mechanism and maintain alignment of the innominate relative to the sacrum in the closed pack position, that is, the innominate would tend to anteriorly rotate relative to the sacrum. The ability of the therapists to show good inter-rater reliability in detecting an altered pattern of intra-pelvic motion suggests that recognition of altered movement patterns is possible. Further research is required to determine the validity and specificity of the Stork Support test in assessment of functional load transfer through the pelvis, and its relevance in clinical practice.
References
1.Schwarzer A, Aprill C, Bogduk N. The sacroiliac joint in chronic low back pain. Spine.1995;20:31-37.
2. Wurff P, Hagmeijer R, Mejne W. Clinical tests of the sacroiliac joint. A systematic methodological review. Part 1: reliability. Manual Therapy 2000; 5:30-36.
3. Vleeming A, Volkers A, Snijders C, Stoeckart R. Relation between form and function in the sacroiliac joint. 2: Biomechanical Aspects. Spine. 1990;15: 133-136.
4. Snijders C, Vleeming A, Stoeckart R. Transfer of lumbosacral load to iliac bones and legs. 1: Biomechanics of self-bracing of the sacroiliac joints and its significance for treatment and exercise. Clinical biomechanics. 1993;8: 285-294.
5. Sturesson B, Selvik G, Uden A. Movements of the sacroiliac joints: a roentgen stereogrammatic analysis. Spine. 1989;14: 162-165.
6. Hungerford B, Gilleard W, Hodges P. Evidence of altered lumbo-pelvic muscle recruitment in the presence of sacroiliac joint pain. Spine. 2003;28: 1593-1600.
7. Vleeming A, Pool-Goudzwaard A, Stoeckart R, etal.The posterior layer of the thoraco-lumbar fascia: its function in load transfer from spine to legs. Spine. 1995;20: 753-758.
8. Hungerford B, Gilleard W, Lee D. Altered patterns of pelvic bone motion determined in subjects with posterior pelvic pain using skin markers. Clinical Biomechanics. 2004;19:456-464.
9. Hungerford B &Gilleard W. Reliability of 3Dimensional motion analysis of sacroiliac joint motion in normal subjects during the stork & hip drop tests. 5th IOC World Congress of Sports Science, Sydney;1999.
10. Maslen B and Ackland T. Radiographic study of skin displacement errors in the foot and ankle during standing. Clinical Biomechanics 1994:9, 291-296.
11. Hodges P, Richardson C. Contraction of the abdominal muscles associated with movement of the lower limb. Physical Therapy 1997:77: 1132-144.
12. Moseley G, Hodges P, Gandevia S. Deep and superficial fibres of multifidus are differentially active during arm movements. Spine 2002: 27: E29-E36
13. RichardsonCA, Snijders CJ, Hides JA, Damen L, Martijn SP, Storm J. The relationship between transversus abdominis muscles, sacroiliac joint mechanics, and low back pain. Spine 2002: 27, 399-405.
14. Willard FH. The muscular, ligamentous, & neural structure of the low back & its relation to back pain. In: Vleeming A, Dorman T, Snijders C, Stoeckart R., ed. Movement, Stability, & Low Back Pain. New York: Churchill Livingstone. 1997. 3-35.
15. Vleeming A, Snijders C, Stoeckart R, et al. A new light on low back pain. 2nd Interdisciplinary World Congress on Low Back Pain, San Diego 1995..
16. Vleeming A, Stoeckart C, Snijders C. The sacrotuberous ligament: a conceptual approach to its dynamic role in stabilising the sacroiliac joint. Clinical Biomechanics 1989: 4: 201-3.
17. Lee D. The Pelvic Girdle: an approach to examination and treatment of the lumbo-pelvic-hip region. Edinburgh: Churchill Livingstone 2004.
18. Hungerford B, Gilleard W, Moran M, Emmerson C. Evaluation of the ability of Physical Therapists to palpate intra-pelvic motion with the stork test on the support side. J Physical Therapy,2007; 87(7): 879-887
19. Pittenger D. Behavioural Research Design and Analysis. New York : McGraw-Hill; 2003.